Archives
Self-Care COPD Program Lowered Hospital Re-admissions
 Self-management of chronic obstructive pulmonary disease (COPD) could significantly reduce the number of hospital readmissions and increase patient quality of life, according to finding of a new study.
Self-management of chronic obstructive pulmonary disease (COPD) could significantly reduce the number of hospital readmissions and increase patient quality of life, according to finding of a new study.
Researchers developed the study at Johns Hopkins Bayview Medical Center, which entailed a three-month BREATHE program combined with transition support and chronic disease self-management. The goal of the study was to determine I if it were possible to improve quality of life and acute care reduction for those suffering from COPD.
COPD encompasses a group of conditions, including emphysema and chronic bronchitis, that causes irreversible lung damage. More than 1 of every 10 seniors have COPD, and 1 of 5 people admitted into the hospital with a COPD exacerbation are re-hospitalized within a month.
According to lead author, Hanan Aboumatar, MD, MPH, associate professor of medicine at the Johns Hopkins University School of Medicine, people with COPD must maintain a “meticulous juggling act: learning about the various medications they must take, how to use multiple inhalers, maintaining the ability to do the activities they enjoy, and recognizing flare-ups early before they get serious enough to warrant a hospital admission.”
In other words, COPD patients must learn extensively about their condition and how to best live with it throughout their daily lives, Aboumatar said. “Unfortunately, patients often report not receiving sufficient information about COPD and how to manage it. Many don’t know how to use their inhalers or how to get portable oxygen devices so they can still leave their home.”
Between March 2015 and May 2016, 240 patients were randomized to receive usual care or intervention care. Usual care patients were assigned a general transition coach who supported the patient for 30 days after discharge, providing guidance with a discharge plan and outpatient services. For intervention care, nurses with specialized training in supporting COPD patients, met with patients during their hospital stay and for three months after discharge.
Hospitalizations, emergency department visits, and the St. George’s Respiratory Questionnaire (SGRQ) quality of life score were monitored for six months after initial hospitalization. For the 203 patients who completed the study, the number of COPD-related acute events was 0.72 for the intervention group and 1.40 in the usual care group.
The SGRQ score for the intervention group decreased by only 1.53 points; however, the score for the usual care group showed a notable rise, at 5.44 points, researchers discovered.
Aboumatar said the COPD patients and caregivers that partnered with their research team to develop the BREATHE program were able to share important information about their needs and what areas healthcare providers needed to focus on. “We are planning to repeat this study in a wider variety of hospitals, including ones in rural settings and those serving patients who have more access to resources,” she added.
The study, “Effect of a Program Combining Transitional Care and Long-term Self-management Support on Outcomes of Hospitalized Patients with COPD," was originally published in JAMA.
Is There An Impact on Lung Cancer Survival because of COPD?
 Lung cancer and chronic obstructive pulmonary disease (COPD) are both diseases that are heterogeneous and diverse, with different pathological changes, clinical manifestations and outcomes for those afflicted by them. So, as researchers investigated the association between COPD phenotypes -- characteristics of an individual resulting from the interaction of its genotype with the environment -- and the prognosis of different types of lung cancer, they found that COPD and emphysema were independent risk factors for squamous carcinoma only.
Lung cancer and chronic obstructive pulmonary disease (COPD) are both diseases that are heterogeneous and diverse, with different pathological changes, clinical manifestations and outcomes for those afflicted by them. So, as researchers investigated the association between COPD phenotypes -- characteristics of an individual resulting from the interaction of its genotype with the environment -- and the prognosis of different types of lung cancer, they found that COPD and emphysema were independent risk factors for squamous carcinoma only.
The researchers had speculated that the diverse nature of the two diseases played an “important role in the relationship between COPD and lung cancer prognosis,” the researchers found.
The study included individuals with a newly and pathologically confirmed diagnosis of lung cancer who were preparing for lung cancer surgery. These individuals also underwent a pulmonary function test and diagnosis of COPD was determined based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) Guidelines.
Of the 2,222 lung cancer patients, 32.6 percent were found to also have COPD. After adjustment for age, sex, body mass index, smoking status and therapy method, COPD was significantly associated with the decreased overall survival of lung cancer. With the increased severity of COPD, the overall survival of lung cancer gradually worsened.
In terms of disease heterogeneity, emphysema was an independent prognostic risk factor for squamous carcinoma, and no significant relationship between COPD and lung cancer prognosis was observed among adenocarcinoma, small cell lung cancer, large cell lung cancer and other subtype patients.
According to AJMC, there have been conflicting results from previous studies about whether or not COPD affects lung cancer survival. The researchers involved with this latest study said that to their knowledge this current study is the largest to date that examines this specific issue.
Unfortunately, per the findings, the five-year overall survival rates of lung cancers with COPD were significantly lower than that of lung cancers without COPD. The results were higher than the overall five-year survival in overall lung cancer population,but were consistent with overall survival rates in patients undergoing surgery
Click here to read the whole article om the AJMC site.
Study Shows that Protein May Slow Emphysema
 A protein generated as part of our body's immune response to intestinal worms could slow the progression of emphysema, Rutgers University found in a recent study, which was published in the journal Cell Reports.
A protein generated as part of our body's immune response to intestinal worms could slow the progression of emphysema, Rutgers University found in a recent study, which was published in the journal Cell Reports.
Past studies have shown that inflammation associated with activated immune cells can contribute to the development of emphysema. The Rutgers study suggests that a protein, RELM-alpha, produced in response to an infection with parasitic worms can suppress the harmful inflammation linked to emphysema and control its progression.
"When the parasite first enters the lungs, it induces production of the inflammatory cytokine IL-17, which can cause emphysema," said William Gause, director of the Center for Immunity and Inflammation at Rutgers New Jersey Medical School, and lead author of the study. "But subsequently the parasite also triggers this specific component of the immune response that can reduce the IL-17 and thereby limit the severity of the emphysema."
Gause said the study is one of many currently examining the immune responses triggered by parasites, which scientists hope will help them identify new treatments to control inflammation and promote lung tissue repair. Studies such as these are looking to identify molecules that may hold potential for actually reducing lung tissue damage.
Future studies, he said, will continue examining whether or not direct administration of this molecule can reduce the severity of emphysema, as well as how harmful inflammation driven by IL-17 results in the immune-mediated tissue damage that contributes to this lung disorder.
"Harmful inflammation is such a serious problem in disease," Gause said. "This protein produced by immune cells during parasitic worm infections reveals the complexity of the immune response and indicates how we can unleash beneficial components of our own immune system to control the harmful inflammation that contributes to many chronic diseases."
Impact of “Seasonal COPD” Reviewed
Patients with chronic obstructive pulmonary disease (COPD) often have a significant disease burden that is particularly associated with the peak incidence of exacerbation events during winter months. Per a review of several existing studies, researchers evaluated the impact of seasonality in COPD, and found that there is indeed important considerations for understanding how all factors of the disease might impact patients and where interventions can be targeted.
The review used the Global Initiative for Chronic Obstructive Lung Disease (GOLD) Guidelines to define a COPD exacerbation as an acute event characterized by “the worsening of a patient’s respiratory symptoms that is beyond normal variation and leads to a change in medication,” the AJMC reports.
Of the studies reviewed, one study showed that its authors demonstrated that the “expression of anti-inflammatory genes was altered by the time of the year -- highly expressed in June, July and August in the northern hemisphere and raised in December, January and February in the southern hemisphere.” Thus, it seems there is a strong correlation for COPD flare ups and environmental factors found in each season.
Additionally, in regard to environmental factors, the authors of the review said that extremes in temperature are typically associated with an increase in morbidity and mortality in the general population. COPD, the reviewers discovered, showed inconsistencies among “a range of study results” in the sample reviewed, reflecting the “complexity of the associations among a variety of environmental factors,” as well as the immune response from the host.
In their review, the authors of the aggregate study said its findings emphasize the need for more research into seasonal CPOD and their effects on those suffering from the illness. In other words, “the biology of a patient in response to seasonality needs to be better understood to provide better treatment and prevention options,” according to the review.
“This seasonal variation in exacerbation incidence has a corresponding effect on hospital admissions in many different healthcare systems and is also associated with an increase in mortality,” the authors said in a statement. “Therefore, a greater understanding of the factors that contribute to these seasonal increases in exacerbation rates should provide opportunities to protect patients and reduce the burden on already-overstretched healthcare systems.
“Research should be undertaken with a clear knowledge of the changing environmental conditions that patients experience,” the authors added. “In this study, we have discussed the factors separately, although, they are all clearly interconnected; importantly, with growing climate extremes, there is a risk that this will impact on seasonal variations in exacerbations rates.”
Click here to read the entire article on AJMC.
Women More Likely To Develop COPD
 A total of 4,484 current and former smokers with COPD from the Genetic Epidemiology of COPD cohort were recently investigated using regression modeling to explore the association between gender, age, disease severity, and the contributing elements of the Global Initiative for Chronic Obstructive Lung Disease (GOLD) classification who were observed across multiple age categories.
A total of 4,484 current and former smokers with COPD from the Genetic Epidemiology of COPD cohort were recently investigated using regression modeling to explore the association between gender, age, disease severity, and the contributing elements of the Global Initiative for Chronic Obstructive Lung Disease (GOLD) classification who were observed across multiple age categories.
Compared to men with COPD, younger women with COPD had a greater likelihood of more severe dyspnea, airflow limitation, greater risk for exacerbations. These differences were less pronounced in older women with COPD. However, older women remained more likely to experience severe dyspnea and to manifest more severe COPD than older men, despite lower pack-years of smoking.
COPD has historically been viewed as a disease of men; however, prevalence and mortality have been increasing in women in recent decades. This has been attributed to increasing rates of smoking among women, and evidence suggests women may be more susceptible to the harmful effects of cigarette smoke and other known COPD risk factors. Gender differences have previously been observed in the clinical manifestations of COPD, with women reporting more severe dyspnea and a higher rate of exacerbations compared to men.
Women and younger patients with COPD tend to report higher levels of physical and psychological symptoms, and women also are over-represented amongst subjects with severe, early-onset COPD. In a study of 2,500 current and former smokers in Genetic Epidemiology of COPD (COPDGene) cohort, females showed an increased the risk of severe early-onset COPD by threefold. The predominance of women with early-onset COPD suggests that younger women may, in general, be more susceptible to severe manifestations of the disease, although more research is needed to clearly define age-by-gender interactions.
Research has begun to explore gender and age differences in the clinical features of COPD; however, no studies have taken a detailed approach to examine gender differences by age across GOLD grades and symptom groups.
The objective of the present study was to explore gender-by-age interactions and disease severity as defined by GOLD groupings and the three key contributing elements of the GOLD classification system (symptoms, exacerbation risk, and airflow limitation severity) using data from a large well-phenotyped COPD cohort.
This study suggests that women are more likely to be significantly burdened by the symptoms of COPD than men, and this effect appears most pronounced among younger women. Although prior results have highlighted important sex and gender differences in men and women with COPD, the modeling of age by gender interactions across the fifth through eighth decades of life is a point of novelty and highlights the clinical imperative to more effectively and thoroughly recognize and manage respiratory symptoms in women.
Study: Emphysema and Heart Failure a Deadly Combination
 In a single-center study of smokers with heart failure, those who also had emphysema identified by CT were twice as likely to be re-hospitalized for heart failure in the following two years, and they demonstrated 70 percent greater odds of dying during that time frame than smokers without emphysema.
In a single-center study of smokers with heart failure, those who also had emphysema identified by CT were twice as likely to be re-hospitalized for heart failure in the following two years, and they demonstrated 70 percent greater odds of dying during that time frame than smokers without emphysema.
The researchers identified 225 inpatients who both smoked and had heart failure from January through March of 2014. The study population was 69 years old on average, 69 percent male and had an average left ventricular ejection fraction (LVEF) of 46 percent. Forty-six percent of those patients had emphysema upon CT. After adjusting for other risk factors, they were 2.11 times more likely to be re-admitted for heart failure over a 2.1-year follow-up and 70 percent more likely to die.
In addition to being more likely to wind up back in the hospital, emphysema patients also averaged longer stays (seven days versus five) and were likely to be re-admitted sooner—a median 162 days versus 327 days for people without emphysema.
“These data should serve as the basis for further study including considering whether therapy based on the presence of emphysema on CT can improve complex HF outcomes,” lead author Puja Kohli, MD, with Massachusetts General Hospital in Boston, and colleagues wrote in PLOS One.
“Our study findings add to that data and show an association between emphysema by CT and an increased cardiac afterload specifically among patients with HF,” they wrote. “The mechanism by which afterload is increased in patients with emphysema and HF is unclear; however, data suggest that increased transmural pressure because of thoracic pressure swings, extrinsic compression in the setting of hyperinflation, and systemic inflammation may all play a role.”
Kohli and colleagues noted that almost half of the patients in their study had emphysema, including 39 percent without known chronic obstructive pulmonary disorder.
“This under-recognized group of patients with both emphysema and heart failure may benefit from improved recognition and characterization of their co-morbid disease processes and optimization of therapies for their lung disease,” the authors wrote.
Click here to read the entire article on Cardiovascular Business.
Patients with COPD Prioritize Symptom Control Information Online
Patients with chronic obstructive pulmonary disease (COPD) still rely on their healthcare providers as the source of primary information about their disease, but about a third of these folks still bring information from the internet and the famous “Dr. Google” to appointments with them to discuss and prioritize information about symptom control, a recent online survey reported.
The research, conducted to understand how patients with COPD perceive web-based health information, was designed to determine behaviors of patients with COPD in use of the internet to learn about their disease; assess their perspectives regarding two educational websites (from the American Lung Association [ALA] and the COPD Foundation); and to see whether patient characteristics, such as older age, severity of breathlessness on the modified Medical Research Council (mMRC), and number of exacerbations in the past year, affected internet health behaviors and assessment of COPD educational websites.
Results from the online survey, completed by 445 respondents, found that physicians were the primary source of information, followed by COPD internet searches; COPD health searches focused on two areas -- specific information about COPD and treatments; patients prioritized disease information in order of “symptom control,” “how COPD affects my body,” and “treatments that might work for me”; attributes of the ALA website were rated mostly higher than the COPD Foundation website.
Ninety-five percent of the respondents said that they rely heavily on their physician as their primary source of information about COPD, but the authors noted that available time for discussions in the office may be limited. Similar to a 2013 Pew Research Center report that found that 72 percent of adult internet users in the United States sought online health information within the past year, 76 percent of these respondents indicated that they performed internet searches about COPD.
Patients rated content of both websites as “good” with mean overall ratings of approximately seven out of 10. Meaning that there is opportunity to improve online materials to achieve higher patients’ ratings. Assessments of specific features indicate that respondents provided higher ratings for all five impression attributes and for eight of nine content attributes on the ALA website compared with the COPD Foundation website. The identities of the websites were hidden during the survey.
Researchers hope that with improved knowledge about a chronic condition like COPD might help patients participate in collaborative self-management plans to improve outcomes. Individuals and organizations can use the findings to modify or enhance information about COPD on their websites. Healthcare providers could also use the survey to help recommend educational websites to patients, they said.
Multiple educational approaches are important to provide both interesting and informative content about COPD on the internet, the study said.
The study has several limitations: the respondents required internet access to participate, so findings may not be applicable to patients without a computer or digital literacy; the respondents were viewing sample static screenshots and not navigating live websites; and only two organizations were selected for review.
Click here to read the entire article on AJMC.
More than 40 Percent of Women with Asthma May Develop COPD
 More than four in 10 women with asthma may eventually develop chronic obstructive pulmonary disease (COPD), according to a study conducted in Ontario, Canada, and published online in the Annals of the American Thoracic Society.
More than four in 10 women with asthma may eventually develop chronic obstructive pulmonary disease (COPD), according to a study conducted in Ontario, Canada, and published online in the Annals of the American Thoracic Society.
In “Asthma and COPD Overlap in Women: Incidence and Risk Factors,” Teresa To, PhD, and co-authors report that of the 4,051 women with asthma included in their study, 1,701 -- or 42 percent -- developed COPD. The woman of the study were followed for 14 years after being diagnosed with asthma, researchers examining risk factors for developing asthma and COPD overlap syndrome, known as ACOS. Those who developed ACOS experience increased exacerbations and hospitalizations and, thus, had a lower quality of life compared to those who have asthma or COPD alone.
The authors also reported that individual risk factors played a more significant role in the development of ACOS than exposure to fine particulate matter, a major air pollutant that because of its microscopic size penetrates deep into the lungs. Also, those women who had a more than five-pack-year smoking history, meaning they had smoked more than the equivalent of a pack of cigarettes a day for five years, were much more likely to develop ACOS than those who smoked fewer cigarettes or never smoked.
Smoking was not the only reason for the development of ACOS, however. Thirty-eight percent of the women who developed ACOS in the study had never smoked.
In addition to smoking, the study identified obesity, rural residence, lower education levels and unemployment as significant risk factors for ACOS. The authors speculated that these factors indicative of low socioeconomic status may result in suboptimal access to care, under-treatment of asthma and poor compliance to medications.
These factors can lead to more frequent attacks of asthma, which can lead to “airway remodeling” that increases the chances of developing ACOS.
“Previous studies have found an alarming rise in ACOS in women in recent years and that the mortality rate from ACOS was higher in women than men,” said Dr. To, a professor in the Graduate School of Public Health at the University of Toronto in Canada. “We urgently need to identify and quantify risk factors associated with ACOS in women to improve their health and save lives.”
The authors of the study said that are “encouraged by the fact that most of the risk factors identified” can be modified.
“The adverse impact of smoking and obesity on health may be even worse in those who are already living with asthma or COPD," said Dr. To. “Identifying modifiable risk factors in the progression from asthma to COPD is an essential first step in developing prevention strategies that lead to a healthy, active lifestyle.”
Black Lung Disease on the Rise
 Black lung disease – known clinically as coal workers’ pneumoconiosis or CWP – that afflicts coal miners in Appalachia is on the rise, the National Institute for Occupational Safety and Health (NIOSH) reports.
Black lung disease – known clinically as coal workers’ pneumoconiosis or CWP – that afflicts coal miners in Appalachia is on the rise, the National Institute for Occupational Safety and Health (NIOSH) reports.
According to NIOSH, the latest national estimate of 10 percent of coal miners with the disease is higher than the estimate last reported using data from 2012. That data showed that just 7 percent of coal miners who worked more than 25 years in underground mines had evidence of black lung.
In just six years, the number of black lung cases in coal miners is up by 3 percent, the organization says. “One in 10 underground coal miners who have worked in mines for at least 25 years were identified as having black lung,” NIOSH said. “Coal miners in central Appalachia (Kentucky, Virginia, and West Virginia) are disproportionately affected with as many as one in five having evidence of black lung – the highest level recorded in 25 years.”
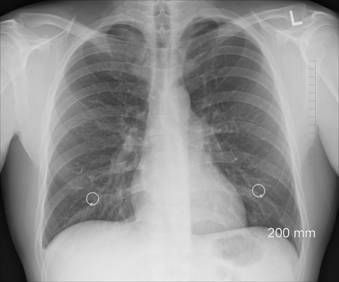
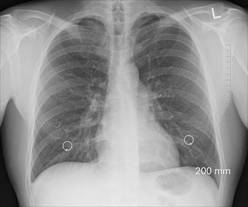
The data is from the Coal Workers Health Surveillance Program (CWHSP). Established in 1970, the CWHSP offers health screening services to miners, including periodic chest X-rays, lung function testing, respiratory health assessment questionnaires and extended health surveillance to workers at surface coal mines.
NIOSH notes that by the late 1990s, the proportion of screened miners with black lung disease reached the lowest level on record.
Lower incidence outside Appalachia
NIOSH research also suggests that there has been a dramatic increase in progressive massive fibrosis (PMF), the most severe form of black lung disease. PMF had fallen to 0.08 percent among all miners examined by NIOSH in the CWHSP in the late 1990s. Miners outside central Appalachia excluded meant “the prevalence for the remainder of the United States was lower, but an increase since 2000 remains evident.”
Increases in the disease may be related to several recent developments, including the use of more sophisticated mining equipment that generates finer dust particles, which exacerbates the onset of disease when they reach the lungs.
Detection, control, screening
Black lung disease is preventable and that “recently enacted protections to prevent coal mine dust exposure and to identify CWP at its early stage remain essential to protect U.S. coal miners.”
Medical screenings should involve both detecting and controlling airborne coal dust. In addition, real-time dust samplers, which include personal dust monitors, have also been approved by the U.S. Mine Safety and Health Administration for use in underground mines.
COPD Sufferers Can Breathe Easier with New App
 There’s an app for that – helping those living with COPD to breathe easier.
There’s an app for that – helping those living with COPD to breathe easier.
The app, Respirate, was created by two high school students in North Carolina and has gone on to win a national contest. The computer company Lenovo announced recently that Respirate is the online “Fan Favorite” as part of its 2018 Lenovo Scholar Network National Mobile App Development Competition.
The app’s most basic function is to help people who have chronic lung diseases improve their ability to breathe. Respirate operates by showing those with COPD how to perform various exercises to help them improve their lung function.
Respirate supplements pulmonary rehabilitation, a program of exercise and education for people who have COPD and other respiratory illnesses. In addition to showing people how to perform various exercises, the app includes to-do lists, reminders and motivational messages, and helps people calculate their body mass index (BMI) to determine how much body fat they have and how they can bring it down.
Possible upgrades include offering Respirate in more languages and seeing whether it can be offered on Apple devices.
Udai Virk and Jeffrey Li, juniors at Enloe High School in Raleigh, developed the app because they know people who have COPD, the third-leading cause of death in the country. “It was extremely mind blowing when we won,” said Virk, 16. “But when we sat down and thought about it afterward, we realized how spectacular our app could be.”
“We thought this was a huge thing,” Li said. “Let’s develop an app to help people manage this.”
The students are members of the Wake County magnet school’s health sciences academy.
Respirate was among six national winners announced in May, leading to the online “Fan Favorite” competition.
The app can be downloaded on the Google Play Store for use on Android devices.
Click here to read the full article on the Raleigh Herald Sun.




