Archives
Unhealthy Lungs Can Lead To Severe Complications From COVID-19
Everyone is susceptible to a COVID-19 infection, but to those living with unhealthy lungs, the virus can be even more harmful. That’s according to a study of more than 1,000 hospitalized patients in China which found that those with chronic obstructive pulmonary disease (COPD) are more than twice as likely to develop severe symptoms from COVID-19. Half of those patients died from the virus or had to be admitted to an intensive care unit and/or put on a ventilator.
“If you add another injury on a system which is already behind, that will put that system in a very dire condition,” says Rabih Bechara, MD, a pulmonologist at the Medical College of Georgia.
Healthy lungs and airways are lined with cilia – small hairs that push phlegm and other secretions out of the lungs and into the throat. But for those living with chronic lung conditions, the cilia are damaged and destroyed, allowing secretions to pile up and constrict airways. Damaged cilia also prevent the lungs from clearing out viral infections such as COVID-19.
“These people tend to collect organisms in their lungs that healthy people clear with a good cough,” explains Jill Ohar, MD, a pulmonologist at Wake Forest Baptist Medical Center in North Carolina.
Some people may have COPD and not even know it. Someone over the age of 40 with a history of smoking and who gets winded after a 10-minute walk could be in the early stages of COPD.
Consequently, it is important to be hyper vigilant and take precautions to stay safe during the COVID-19 pandemic. Among those precautions are maintaining social distance, limiting trips to the store or getting your groceries delivered, and seeing physicians via phone or video rather than going into the office.
Wear a facemask when leaving the house. And, if you do get sick, make sure you have enough medication for at least two weeks.
Read the full article here from Health Central.
COVID-19 Poses Serious Risk to People With COPD, Asthma
People living with chronic pulmonary obstructive disorder (COPD), asthma or other chronic lung diseases should take extra precautions during the COVID-19 pandemic, according to experts from the American Lung Association.
"Everyone's health is at risk from COVID-19, and those living with a lung disease or who are immunocompromised may be more vulnerable to the impacts of the virus," said Dr. Albert Rizzo, the association's chief medical officer.
To protect themselves from COVID-19, which can cause a pneumonia-like lung infection with a range of symptoms from mild or absent in some to life-threatening in others, Rizzo said it is important for people with chronic lung diseases to take their medications while keeping their healthcare provider updated about any symptoms or changes in their health. This includes patients with lung cancer whose immune systems may be compromised.
Social distancing – maintaining 6 feet between yourself another person – is one way to lessen the chances of getting infected with COVID-19. Other measures include washing your hands for at least 20 seconds, avoiding touching your face, nose and mouth and, perhaps most importantly, avoiding contact with people who have contracted the virus.
“It’s important for those with lung disease to use their best practices in managing their disease,” Rizzo said.
Chronic lung disease isn’t the only condition that can lead to complications from COVID-19. Cigarette smokers, including people who vape and use e-cigarettes, are also at an increased risk, Rizzo said.
"Cigarette smoking and vaping are linked to lung inflammation and lowered immune function in the lung's airways, both of which can increase the likelihood of complications if exposed to COVID-19," he said. "Therefore, long-term smokers and e-cigarette users may have a higher risk of developing chronic lung conditions associated with severe cases."
Access the full article here from Web MD.
More studies link vaping to asthma and COPD
 Although studies cannot definitively prove a link between the use of electronic cigarettes and asthma and chronic obstructive pulmonary disease (COPD), lung illnesses and deaths from vaping continue to make headlines—and two recent studies show potential evidence of the practice's long-term respiratory concerns.
Although studies cannot definitively prove a link between the use of electronic cigarettes and asthma and chronic obstructive pulmonary disease (COPD), lung illnesses and deaths from vaping continue to make headlines—and two recent studies show potential evidence of the practice's long-term respiratory concerns.
The new studies connect the use of e-cigarettes to asthma and COPD, adding "to the body of evidence on the relationship between electronic cigarette use and lung conditions,” said Dr. Albert Osei, a post-doctoral fellow at Johns Hopkins University School of Medicine in Baltimore, who was the lead author of a study published in the American Journal of Preventive Medicine.
The studies cannot prove a cause-and-effect link, but the results suggest that “further longitudinal studies" are required, he added.
E-cigarettes have been marketed for more than a decade as being less harmful than traditional tobacco cigarettes, and as a solution for helping people quit smoking. In 2016, they were used by nearly 11 million American adults.
Previous studies show that vapor may irritate airway cells, impair their ability to fight infection, and lead to the destruction of lung tissue. Other studies have shown that e-cigarette users are at significantly higher risk of chronic lung diseases, including asthma, bronchitis, emphysema, and COPD. Since January 7, 2020, there have been more than 2,600 illnesses and 57 deaths linked to vaping products with THC, the component in marijuana that produces a high.
Osei's study examined a database of more than 705,000 adults. About 65,000 smoked regular cigarettes and more than 25,000 smoked e-cigarettes. The average age was between 30 and 34 and more than 200,000 were previous smokers. Among the findings:
- 53,000 said they had COPD, chronic bronchitis, or emphysema
- E-cigarette use was associated with 75% higher odds of COPD among those who had never smoked tobacco cigarettes
- Daily e-cigarette users had a 2.6 times higher likelihood of COPD than people who never smoked cigarettes.
A second study – published in the journal BMC Pulmonary Medicine – had more than 400,000 adults who never smoked cigarettes. More than 34,000 had asthma; 3,100 people currently use e-cigarettes. Their average ages were 18 to 24. The risk of asthma was 39% higher in current e-cig users than in people who never vaped. The more they vaped, the higher their asthma odds.
Study author Osei pointed out that both combustible and e-cigarettes contain nicotine.
For more information about the study, visit Health 24.
Vitamin D Deficiency Associated with Worsening Lung Function in COPD
 Researchers have found that, in patients with chronic obstructive pulmonary disease (COPD), a deficiency in vitamin D may be associated with worsening lung function and disease exacerbations.
Researchers have found that, in patients with chronic obstructive pulmonary disease (COPD), a deficiency in vitamin D may be associated with worsening lung function and disease exacerbations.
According to study results published in CHEST, samples from more than 1,600 patients with COPD who participated in a previous study were included in this analysis. All were current or former smokers, and between ages 40 and 80 years.
Researchers assessed the levels of vitamin D and categorized samples as either being deficient or not. The samples collected predicted forced expiratory lung volume in one second with COPD exacerbations the primary outcomes of interest. Based on these findings, vitamin D deficiency was found in more than 20% of those in the study.
Prevalence of the vitamin D deficiency was highest in those who were younger; active smokers (48% vs. 30%), and black participants (29% vs. 10%). Participants with vitamin D deficiency had a significantly lower post-bronchodilator percent.
The takeaway: a vitamin deficiency may impact the level at which COPD develops.
For more information about the report, see the complete story on Pulmonary Advisor.
COPD Prevalence, Diagnosis, and Mortality: Differences Between Women and Men
 Women were more likely than men to be diagnosed with chronic obstructive pulmonary disease (COPD), and had more frequent exacerbations, according to the results of a Swedish study published in the Nature Partner Journal Primary Care Respiratory Medicine.
Women were more likely than men to be diagnosed with chronic obstructive pulmonary disease (COPD), and had more frequent exacerbations, according to the results of a Swedish study published in the Nature Partner Journal Primary Care Respiratory Medicine.
The incidence of COPD, prevalence of asthma and other comorbidities, exacerbation risk, mortality rate, COPD-related prescriptions, and healthcare resource use were retrospectively analyzed from a large, real-world, retrospective cohort study conducted in Swedish patients with COPD.
Differences between these outcomes and sex were compared between groups.
Over the past 50 years, the prevalence of COPD among women in the United States has sharply increased. Now, COPD afflicts and kills more women than men.
“Things like breast cancer get a lot of attention, but we have many more women die of COPD every year,” Dr. MeiLan Han, MS, an associate professor of medicine in the Division of Pulmonary and Critical Care Medicine at the University of Michigan and a volunteer spokesperson for the American Lung Association, recently told Healthline.
More than 7 million women in the United States are living with a diagnosis of COPD — and many more may have the condition without realizing it.
“There is some evidence that suggests women may actually be more susceptible to the effects of tobacco smoke,” Han explained. “For each cigarette smoked, the amount of function loss seems to be greater [for women]. One theory is that it’s because the lungs of women are smaller. If you can imagine, one cigarette is a larger effective dose in women versus men.”
According to the Nature Partner Journal Primary Care Respiratory Medicine, among the 101,934 medical records available, 17,479 patients were diagnosed with COPD. Among those with COPD, 54.4% were women and 45.6% were men.
The prevalence of asthma was higher in women (12.3% vs 9.4%), and women also had more frequent exacerbations than men; in fact, women had 12% higher risk for an earlier exacerbation vs. men. However, the mortality rate was found to be significantly higher in men, as women lived an average of two years longer than men from COPD diagnosis to death.
“Despite a lower mortality rate, women had higher prevalence [of] comorbidities including asthma and a higher risk of exacerbations, leading to more utilization of COPD drugs and COPD-related healthcare resources,” the researchers wrote. “In daily clinical practice, healthcare professionals in primary care play a pivotal role and should consider all these parameters in order to properly diagnose and treat women with COPD.”
For more information regarding the study, read the article on Pulmonology Advisor.
COPD mortality rates declining, but total deaths increasing
 COPD mortality rates have declined from 1995 to 2017 in many countries. Still, the total number of deaths attributable to COPD has increased during the past 20 years, according to new data published in the European Respiratory Journal.
COPD mortality rates have declined from 1995 to 2017 in many countries. Still, the total number of deaths attributable to COPD has increased during the past 20 years, according to new data published in the European Respiratory Journal.
The existing COPD mortality data were based on outdated statistics from a select number of high-income countries in Europe, Australia, Japan and the U.S., says Joannie Lortet-Tieulent, Ph.D., a research fellow at the WHO International Agency for Research on Cancer.
Using COPD data recorded from 1995 to 2017 from the WHO mortality database, the researchers evaluated death counts according to age, sex, and year. Nearly 3.36 million COPD deaths from 24 countries were included in the analysis.
The researchers calculated COPD death rates by comparing the number of COPD deaths per year against the population of each country in the same year and standardized the data using a reference population. Additionally, they restricted their analysis to people aged 50 to 84 years.
Results revealed a 12% decrease — from 68 deaths per 100,000 person-years to 60 deaths per 100,000 person-years — in the combined COPD death rate for all countries from 2000 to 2015. But there also was a 12% increase in the number of total deaths for all countries from 180,950 to 203,090 estimated total COPD deaths.
Researchers think data suggests that the proportion of COPD patients who are dying early because the disease is falling overall, which is encouraging. Perhaps people are less exposed to COPD risk factors now, and that COPD is being managed more effectively.
Despite the general trend toward lower COPD mortality rates in 18 of the 24 countries examined during the study period, mortality rates overall were still twice as high in men than in women. The exceptions were in the United States, New Zealand and the United Kingdom, where rates were similar for both sexes.
“Our study does not explain why COPD death rates among women increased or remained stable in some countries, but we think this trend could be linked to the rise in the uptake of smoking among women over successive generations, as smoking is an important risk factor for COPD,” Lortet-Tieulent said. "In the countries where women have been smoking as much and for as long as men, such as the U.S., New Zealand, and the U.K., the female COPD death rate became very similar to that of men over time."
The researchers noted, though, that their results likely underestimate the burden of COPD mortality and that more data from low-income countries are necessary.
For additional information detailed in the report, visit Healio.
Provider Intervention Leads to Increased Flu Vaccination Rates Among Patients With COPD
 Physician and nurse interventions are the most effective means of promoting influenza vaccinations among patients with chronic obstructive pulmonary disease (COPD), according to the results of a pilot project. Conducted at the National University Hospital in Singapore, the project is the most extensive prospective study of its kind aimed at increasing vaccination rates in patients with COPD.
Physician and nurse interventions are the most effective means of promoting influenza vaccinations among patients with chronic obstructive pulmonary disease (COPD), according to the results of a pilot project. Conducted at the National University Hospital in Singapore, the project is the most extensive prospective study of its kind aimed at increasing vaccination rates in patients with COPD.
The influenza virus, rhinovirus, and respiratory syncytial virus are the most common viral infections among patients with COPD.
Of the 348 participating patients, researchers found the initial baseline vaccination rate to be more than 47% while the final rate was nearly 81%. They also found that regular flu vaccinations reduced COPD exacerbations, which are one of the leading causes of hospitalizations around the globe and carry a mortality rate as high as 20%. In the United States, vaccination rates among people with COPD range between 20% and 60%.
To lower the number of people who did not receive their vaccination and decrease rates of infective exacerbations, researchers collected data from one of Singapore’s tertiary referral hospitals. Patients with COPD were enrolled in an “integrated nurse-led, specialist-supported” program called TAP. The program started in 2013 and researchers followed up with patients in 2015.
Physicians and nurses used various tactics to boost immunization rates. For example, physicians explaining the importance of immunizations and, in some cases, nurses following up with those who didn’t get their vaccinations. Patients and providers also completed surveys and questionnaires distributed at the time of vaccination to determine which intervention methods were the most successful.
Physician intervention accounted for nearly 88% of the increase in vaccinations, with the remaining increase due to nurse reminders.
Researchers said local settings might contribute to the findings. Influenza vaccination awareness is low in Singapore. Those with COPD also were older and had poor health literacy. Also, because doctors knew patients’ vaccination rates would be monitored during the study, physicians consciously made an effort to address the issue, which may have improved the rates of vaccinations.
For additional information about the study, visit AJMC.
Review Suggests Combining Approaches for Identifying COPD
 A review evaluating the methodological approaches of identifying chronic obstructive pulmonary disease (COPD) found that when more criteria are combined, the detection of CPOD is more accurate in terms of sensitivity and specificity.
A review evaluating the methodological approaches of identifying chronic obstructive pulmonary disease (COPD) found that when more criteria are combined, the detection of CPOD is more accurate in terms of sensitivity and specificity.
Researchers conducted a systematic literature review of data from January 2000 through October 2018 using Medline via PubMed and Google Scholar. A manual review of the collected studies was then conducted with at least two independent raters.
In total, 151 publications were assembled and reviewed. Following the title and abstract screening, 39 papers were assessed. The most frequently used criteria set to identify COPD patients included the International Classification of Diseases (ICD) codes, hospitalization, and ambulatory visits.
“In general, it can be concluded that the more criteria are combined, the more accurate is the detection of COPD patients in terms of sensitivity and specificity. Drug data is by far the most comprehensive source of information if used alone,” concluded the authors.
Click here to read to the full article on AJMC.
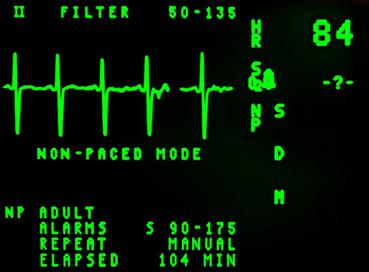
Study Examines Cardiovascular Disease Impact in Patients With COPD
 Cardiovascular disease is often associated with chronic obstructive pulmonary disease (COPD). A recent study investigating the relationship between cardiovascular and COPD symptoms shows there may be a link between a patient's diagnostic status and those of patients with suspicious echocardiographic findings, if these symptoms were undiagnosed and untreated.
Cardiovascular disease is often associated with chronic obstructive pulmonary disease (COPD). A recent study investigating the relationship between cardiovascular and COPD symptoms shows there may be a link between a patient's diagnostic status and those of patients with suspicious echocardiographic findings, if these symptoms were undiagnosed and untreated.
https://pixabay.com/users/reaperdz-3530416/ " >The research was published in the International Journal of Chronic Obstructive Pulmonary Disease. Lung function data was collected including forced expiratory volume in 1 second (FEV1) and echocardiographic data on the left ventricular ejection fraction (LVEF) and end-diastolic diameter (LVEDD).
Researchers note that diagnosis of the predominant underlying disease and its contribution to COPD symptoms is a challenge, a situation complicated by the fact that even when objective measures of heart function are available, they do not necessarily correlate with the magnitude of symptoms.
“Patients may receive cardiovascular medication, which may alleviate symptoms to a variable degree, depending on the type and severity of cardiac disease … [but] the indication that led to medication in the past might not be verifiable at a later time.”
More than 1,590 patients were evaluated in the study, with 289 showing signs of ischemic heart disease, myocardial infarction or heart failure. Another 860 received at least one cardiovascular medication. Of the 948 patients without isolated hypertension, 38% had LVEF less than 50% and 53.4% with LVEDD greater than 56 mm, who lacked cardiac diagnosis and medication.
“The present study revealed a substantial prevalence of cardiac disease in patients with stable COPD. At least one of the three selected cardiac disorders were reported by about one-fifth of the patients, while the rate of suspicious echocardiographic left heart findings was lower. The overlap between reported cardiac history and abnormal echocardiography was low, and only a minority of patients with a respective history exhibited an impaired left ventricular systolic function or dilatation,” researchers wrote.
Researchers now suggest that the direct assessment of heart size and function is likely to be more reliable in the detection of concomitant cardiac disease in COPD patients.
Emphysema Frequently Found During Cancer Screening
 Emphysema that’s detected using lung-density analysis software during low-dose CT lung cancer screening can be highly predictive of lung cancer risk, new research shows.
Emphysema that’s detected using lung-density analysis software during low-dose CT lung cancer screening can be highly predictive of lung cancer risk, new research shows.
The prevalence is about 60%, but "we don't know the threshold at which we should act on the emphysema," researchers said.
https://pixabay.com/users/publicdomainpictures-14/" >Despite such high numbers, it’s not clear how physicians should proceed when it is detected. At this point, because the findings are freshly discovered, there are no current care protocols for how to proceed.
However, that doesn’t mean that the discovery is not important. The screening results may indicate a higher risk for malignancy associated with a higher incidence of cancer. Of these, folks, more severe emphysema is detected in these patients.
The research, led by the Cleveland Clinic lung cancer screening program, uses automated lung density analysis software to detect emphysema. The findings were presented at the American Thoracic Society 2019 International Conference in Dallas.
Researchers said caregivers and the healthcare community must better understand which patients should see a pulmonologist and be treated based on such a test.
For specifics about the screening, emphysema was detected in 125 (39%) of the 321 individuals reviewed. In the study cohort, 101 (31%) participants had previously been diagnosed with chronic obstructive pulmonary disease (COPD).
During the 12-month follow-up, patients with emphysema detected made more pulmonary outpatient visits than patients without emphysema (43% vs. 27%), and were more frequently prescribed treatment for COPD (47% vs. 25%). The rate of visits to the emergency department was similar in the emphysema and no-emphysema groups (35% vs. 30%), as was the rate of hospitalization (7% vs. 12%).
"Patients with emphysema detected had more outpatient visits and more need for inhalers," Choi reported,” investigator Humberto Choi, MD. "We need to better understand which patients should see a pulmonologist and be treated.”
Emphysema was also associated with a higher incidence of lung nodules in a separate study presented by the same team. Their analysis of 314 patients from the same Cleveland Clinic cohort assessed Lung-RADS assessment categories. Five patients were diagnosed with lung cancer during the four-year follow-up period.




