Archives
Those with Lung Disease Still Need to Wear A Mask
 People with chronic lung conditions may be fearful of wearing a mask. But as the United States continues to struggle to contain COVID-19, medical experts say doing so is the right decision as they are at a high risk of becoming severely ill if infected.
People with chronic lung conditions may be fearful of wearing a mask. But as the United States continues to struggle to contain COVID-19, medical experts say doing so is the right decision as they are at a high risk of becoming severely ill if infected.
Everyone, including individuals whose breathing is compromised due to asthma or chronic obstructive pulmonary disease (COPD), should be able to wear non-N95 face coverings without affecting oxygen or carbon dioxide levels. And they need to do so as infections continue to surge across parts of the country.
Experts suggest that those who are worried about wearing a mask should speak with their physician who can mitigate their concerns. Also, try a variety of different facial coverings to find one that is both effective and comfortable.
As the virus continues to spread, the U.S. Centers for Disease Control and Prevention (CDC) recommends wearing masks when out in public, and many states, cities and retail stores have passed their own mandates regarding facial coverings. Experts, however, have instructed the public not to use N95 face masks to ensure that there are enough for healthcare workers.
Along with masks, the most effective ways to help prevent a COVID-19 infection is through social distancing and consistent hand-washing.
The full story can be found here.
FDA Designates Targeted Lung Denervation System as “Breakthrough Device”
 A Minnesota-based company announced that its targeted lung denervation system designed to help patients suffering from chronic obstructive pulmonary disease (COPD) has been designated as a breakthrough device by the U.S. Food and Drug Administration.
A Minnesota-based company announced that its targeted lung denervation system designed to help patients suffering from chronic obstructive pulmonary disease (COPD) has been designated as a breakthrough device by the U.S. Food and Drug Administration.
The AIRFLOW-3 system from Nuvaira Inc. is designed to reduce moderate to severe COPD for patients on optimal medical care. It is a targeted lung denervation system that involves a catheter-based bronchoscopic procedure to disrupt pulmonary nerve input to the lung and reduce clinical consequences of neural hyperactivity. Once in place, the catheter delivers radiofrequency energy to the nerves located on the outside of the airways.The breakthrough device designation came after the FDA reviewed the safety data the first 50 patients enrolled in the AIRFLOW-3 pivotal clinical trial and subsequently granted full investigational device exemption approval to proceed with the full 400-patient study. The trial was approved by the Centers for Medicare and Medicaid Services in April for purposes of Medicare coverage.
“We support our global pulmonary thought leaders who are working hard to ensure patient access to routine care and to important clinical trials like AIRFLOW-3,” said Dr. Dennis Wahr, CEO of Nuvaira, “while simultaneously adapting to the new reality of COVID-19.”
With both the designation and CMS approval in place, the AIRFLOW-3 pivotal trial is now enrolling participants with COPD aged 40 to 78 years. Participants will be randomly assigned to targeted lung denervation plus optimal medical care or a sham procedure with optimal medical care only.
Read the full story here.
Stem Cell Therapy Provides Hope to COPD Sufferers
 There is no know cure currently for chronic obstructive pulmonary disease (COPD). But studies have shown that stem cell therapy may be able to make life better for those suffering from the illness.
There is no know cure currently for chronic obstructive pulmonary disease (COPD). But studies have shown that stem cell therapy may be able to make life better for those suffering from the illness.
According to astudysponsored by the Lung Institute, 82% of COPD patients who received stem cell treatments, during which stem cells were administered intravenously to find damaged tissues around organs, reported improvements such as increased lung capacity as well as the ability to walk.
Stem cells can change into any cell in the body and are effective against COPD because they can repair damaged lung tissue. This helps minimize chronic breathing conditions such as emphysema or bronchitis. Stem cells are also anti-inflammatories that can help clear airways.
According to the World Health Organization, 65 million people have been diagnosed with moderate to severe COPD, and The American Lung Association lists it as the third-leading cause of death in the United States.
While stem cell therapy doesn’t cure COPD, it has been shown to improve the quality of life in those who have it. It’s a viable option compared to more extensive and expensive options such as total lung transplants.
For more on the story,click here.
How Asthmatics Can Stay Safe During the Pandemic
While there is no clear evidence of COVID-19 having a severe effect on asthmatics, the Center for Disease Control says that people with moderate to severe asthma may be at a higher risk of getting sick if they contract the virus.
“Patients with underlying conditions that specifically involve their lungs, like asthma, COPD, and chronic bronchitis, seem to be more at risk to develop pneumonias and the dreaded acute respiratory syndrome associated with COVID-19,” said Dr. Maruicio Heilbron, a trauma surgeon and vice chief of staff at St. Mary’s Medical Center in Long Beach, California.
There are things asthma sufferers can do to keep themselves safe during the pandemic, beginning with using their inhaler daily as prescribed.
“This will help decrease their risk of an asthma attack triggered by any respiratory virus, including coronavirus,” said Dr. Jonas Nilsen, co-founder of Practio, a travel vaccination and infectious disease advice specialist service.
Albuterol inhalers are being used in hospitals to help COVID-19 patients and are in short supply. It’s a good idea for asthmatics to work with their physician, pharmacist and insurance companies to create an emergency supply of prescriptions, especially if the quarantine continues longer than predicted.
Because they are at a higher risk, people with asthma may be stressed during the pandemic, and anxiety can bring on asthma attacks. There are many coping mechanisms to deal with the stress, such as healthy eating, exercise and meditation. During periods of isolation, it is also important to reach out to family and friends, whether by phone or online.
For more on this story, follow the link.
New hope for COPD patients possible with in-home device
 Researchers say that there may be benefits of in-home non-invasive ventilation therapy for many patients with chronic obstructive pulmonary disease (COPD). Researchers said there are several benefits, including lower mortality, fewer hospital admissions, lower risk of intubation, improved shortness of breath, and fewer emergency department visits.
Researchers say that there may be benefits of in-home non-invasive ventilation therapy for many patients with chronic obstructive pulmonary disease (COPD). Researchers said there are several benefits, including lower mortality, fewer hospital admissions, lower risk of intubation, improved shortness of breath, and fewer emergency department visits.
A study by Mayo Clinic researchers, published February 4, 2020 in JAMA, looked at the use of a non-invasive ventilation or a machine with a mask that helps to improve breathing to treat chronic hypercapnia, a condition impacting many of the 15 million COPD sufferers. Hypercapnia, which is the retention of carbon dioxide may lead to acute respiratory failure and hospitalization.
“Although there is ample evidence supporting in-hospital use of breathing devices such as (bilevel positive airway pressure) BiPAP, until now, we didn't know which benefits may be available when we send people home with a new piece of equipment. There were indications that at-home therapy might be beneficial, but there were conflicting studies and guidelines as to what would be best for our patients,” said Michael Wilson, M.D., a pulmonary and critical care physician at Mayo Clinic, who led the study.
Wilson’s team combined all available peer-reviewed and other expert literature for relevant randomized clinical trials and comparative observational studies. They reviewed more than 6,300 citations, finding 33 studies evaluating outcomes for 51,085 patients with COPD. What they found was that the use of a non-invasive ventilator device led to fewer emergency department visits and hospitalizations, and lower rates of intubation if patients were admitted to the hospital.
While some studies showed better quality of life, other studies showed no difference. Patients with COPD should talk with their physicians to determine whether a breathing device, such as a BiPAP machine, might be the right choice for them.
For more information about the study, visit Science Daily.
Some Patients with Severe COPD Will Improve on Ventilation
 Non-invasive ventilation is a well-known life-sparing option during acute exacerbations of chronic obstructive pulmonary disease (COPD). Still, its effectiveness for severe but stable conditions has been challenging to establish.
Non-invasive ventilation is a well-known life-sparing option during acute exacerbations of chronic obstructive pulmonary disease (COPD). Still, its effectiveness for severe but stable conditions has been challenging to establish.
European studies showed that, in some patients, reductions in chronically elevated carbon dioxide and delivery of high-pressure support allowing the diaphragm to rest contribute to the ventilation effectiveness.
"European data are showing that we need to do things differently," said Lisa Wolfe, MD, from Northwestern University in Chicago. "The new thrust is to do two things," she told Medscape Medical News.
In a recently published review in Annals of the American Thoracic Society, researchers looked at studies of non-invasive ventilation in COPD patients to understand why some saw a benefit and others didn't. The study did not evaluate the "right treatment" in the "right patients," rather, "they were looking at relatively low-level pressure support; we see that levels between 8 mL/kg and 12 mL/kg did not show a benefit," said Wolfe.
She explained that low inspiratory pressure support doesn't "get rid of carbon dioxide. And without successfully doing this, we can't get these people better."
Click here to read the full article on Medscape.
Success! Orlando Health Offers New Lung Valve Treatment for Patients with Severe Emphysema
 Breathing is becoming easier for emphysema patients at Orlando Health Orlando Regional Medical Center (ORMC).
Breathing is becoming easier for emphysema patients at Orlando Health Orlando Regional Medical Center (ORMC).
The health system is the first in Central Florida to offer a new lung valve treatment for patients with severe emphysema, a progressive and life-threatening form of chronic obstructive pulmonary disease (COPD).
The Zephyr Endobronchial Valve System is the first minimally invasive device approved by the U.S. Food and Drug Administration (FDA) to help emphysema sufferers breathe with ease, without major surgery.
The one-time treatment is done during a basic bronchoscopy, which is a procedure that allows doctors to examine a patient’s lungs and air passage, but requires no cutting or incisions.
During the procedure an average of four small valves are placed in the airways to block off the diseased parts of the lungs where air gets trapped. Doing so allows the healthier parts of the lungs to expand and take in more air. This results in patients being able to breathe easier and have less shortness of breath.
According to us, the National Emphysema Foundation, an estimated 3.1 million Americans have been diagnosed with emphysema. Prior to the new valve treatment, emphysema management included medication, oxygen therapy, major surgery, or lung transplant.
The Zephyr Endobronchial Valve treatment was granted Breakthrough Device designation by the FDA based on positive clinical data from the pivotal LIBERATE Study and two other multicenter randomized control trials. Orlando Health ORMC was a site in the LIBERATE Study.
“The endobronchial valve system is a significant advancement for patients with severe emphysema, said Mark A. Vollenweider, MD, MPH, FCCP, interventional pulmonologist, and section chief, Pulmonary Medicine, Orlando Health ORMC. “The valve treatment improves patients’ quality of life by allowing [them] to breathe easier, be less short of breath, and be more active and energetic.
Vollenweider points to two success stories to illustrate the efficacy of the new treatment. One patient who previously was unable to walk from car to office is now traveling overseas, while another has been able to resume a hobby after emphysema forced its abandonment years ago.
“Whether returning to work, enjoying retirements, or celebrations in between, the outcomes have been life changing for our patients," Vollenweider added. "We are honored to have been part of the research that led to the groundbreaking treatment options for patients.”
Poor Sleep Quality Linked to COPD Exacerbations
 Fresh assessments from the Canadian Cohort Obstructive Lung Disease (CanCOLD) seem to suggest that patients with worsened metrics for baseline sleep quality are at a greater risk of long-term chronic obstructive pulmonary disease (COPD) exacerbations.
Fresh assessments from the Canadian Cohort Obstructive Lung Disease (CanCOLD) seem to suggest that patients with worsened metrics for baseline sleep quality are at a greater risk of long-term chronic obstructive pulmonary disease (COPD) exacerbations.
Investigators from McGill University in Montreal led a new study, which provides an ongoing analysis of more than 2,000 random subjects from Canada with mild to severe COPD. The research is designed to better understand the characterizations of the chronic pulmonary condition, and how patient response may influence of individual factors.
Per the report, previous trials associated with COPD showed an increase of sleep disturbance. This can exacerbate the notion that poor sleep quality may also drive an increased rate of respiratory symptoms in patients.
When evaluating the relationship between sleep quality and COPD exacerbation, researchers reviewed data from 480 participants who had completed an 18-month follow-up assessment period. Sleep quality was measured using patient Pittsburgh Sleep Quality Index (PSQI) and three-factor scores at baseline.
Researchers also reviewed symptom-based and event-based exacerbations, including dyspnea, sputum change, and medication or unscheduled health services uses. Of the 480 patients, 185 had at least one exacerbation during the 18-month follow-up, and 203 were found to experience poor sleep quality.
Investigators concluded baseline poor sleep quality increased patient risk for COPD exacerbation over at least 18 months. Thus, treating comorbid sleep conditions could result in reduced exacerbations, benefiting the patients’ respiratory and sleep health.
Emphysema Frequently Found During Cancer Screening
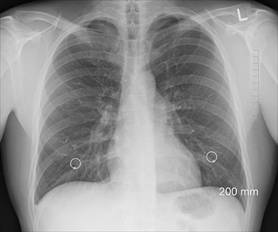 Emphysema detected with lung-density analysis software during low-dose CT lung cancer screening can be highly predictive of lung cancer risk, new research shows.
Emphysema detected with lung-density analysis software during low-dose CT lung cancer screening can be highly predictive of lung cancer risk, new research shows.
“Almost everyone has an incidental finding,” said investigator Humberto Choi, MD, from the Cleveland Clinic, noting that coronary artery disease, renal cell carcinoma and arthritis are all commonly found. “But emphysema is the one we’re concerned about.”
The prevalence is about 60 percent, but because “we don’t know the threshold at which we should act on the emphysema,” it is not clear how to proceed when it is detected, Choi told Medscape Medical News.
No protocol or care path exists, which is important because screening results that fall into categories that indicate higher risk for malignancy are associated with a higher incidence of cancer. Too, more severe emphysema tends to be detected in these patients.
Emphysema was detected in 125 (39 percent) of the 321 participants screened, indicated by a score that was greater than 0 percent. In the study cohort, 101 (31 percent) participants had previously been diagnosed with chronic obstructive pulmonary disease (COPD).
During the 12-month follow-up period, patients with emphysema detected made significantly more pulmonary outpatient visits than patients without emphysema (43 percent vs. 27 percent). The rate of visits to the emergency department was similar both groups (35 percent vs. 29 percent), as was the rate of hospitalization (7 percent vs. 12 percent).
“Patients with emphysema detected had more outpatient visits and more need for inhalers,” Choi said, adding that follow-up and treatment protocols are needed. “We need to better understand which patients should see a pulmonologist and be treated.”
Emphysema also was associated with a higher incidence of lung nodules in a separate study presented at the meeting by the same team. Their analysis of 314 patients from the same Cleveland Clinic cohort assessed Lung-RADS assessment categories. Five patients were diagnosed with lung cancer during the four-year follow-up period.
“The emphysema itself causes benign risk nodules to look different, more irregular,” Choi said.
Lifestyle Changes to Ease the Effects of Lung Disease
 Those affected by COPD are likely to be told by their doctor that there are a number of lifestyle changes they can make to slow the progression of the disease, which has no current cure. Many of these actions are small alterations to their daily lives that can have a positive impact.
Those affected by COPD are likely to be told by their doctor that there are a number of lifestyle changes they can make to slow the progression of the disease, which has no current cure. Many of these actions are small alterations to their daily lives that can have a positive impact.
The following tips are offered by Dr. David Samadi, chief of robotic surgery at Lenox Hill Hospital, and medical contributor for the Fox News Channel’s Medical A-Team. They provide several key factors for helping improve the lives of those living with COPD, helping them breathe easier while slowing the condition
Clean your house – regularly: Dust, secondhand smoke and fumes from paint or other household chemicals are all irritants to lungs. Cleaning your house regularly helps reduce the irritants that make COPD worse. The activity also allows you to get a little exercise. Too, never let anyone smoke in your home. No only does that not come out easily, it’s horrible for your health.
Get some exercise: Before you even begin any sort of exercise routine – even cleaning your house – consult with your doctor, who is likely to encourage you to participate in activities that aren’t too strenuous. Regular exercise typically helps reduce symptoms of depression and may even give you energy than without it. But don’t overdo it, because too much exercise can be dangerous. Take physical activities at a slow pace at least three to four times each week.
Lose weight and stop drinking soda: In line with any exercise, attempt to lose weight by putting a stop to drinking unhealthy soda and other non-nutritious foods. According to Dr. Samadi, “weight gain can be one side effect of consuming soda, but another effect of carbonated beverages is stomach swelling. As your stomach expands, it pushes up against your diaphragm, making it harder to breathe.” Thus, choose healthier beverages, such as water, unsweetened tea, green tea or even coffee.
Stay hydrated – with water: Drink lots of water. Remaining well-hydrated is crucial to managing COPD. Without enough water, “your mucus can become thick, sticking to your lung and adding to the burden of being able to breathe well,” Dr. Samadi says. Try to drink between eight to 10 cups of water daily.
Make healthy food choices: Maintaining a healthy diet is essential. Eating junk food contributes to weight gain, which leads to trouble breathing and slows your ability to exercise. Junk food is also usually loaded with salt, which causes fluid retention resulting in congestion that can obstruct breathing. Choose fruits, vegetables, whole grains, low-fat dairy, nuts and seeds, beans, seafood and lean sources of poultry and beef. Doing so will likely lead to you enjoying your food more, too, as it likely tastes better.
Keep your oxygen with you: Wherever you go, your oxygen tank needs to go too—don’t leave home without it. Low oxygen levels can put an extreme strain on the heart, and the perception of a lack of oxygen can create a tremendous amount of mental and physical stress, which can lead to poor choices.
COPD is a chronic lung condition so it can be challenging and stressful to deal with. Meeting regularly and talking with others who have COPD can help you feel less alone. Sharing your feelings and experiences, and hearing others’ thoughts, can teach you better ways to cope with your chronic condition.




