Archives
Patients with COPD Require More Care than Elderly Heart Failure Patients in a Hospital-based Home Care Setting
 The elderly population is rapidly growing, while lifespans also increase. At the same time, the prevalence of chronic obstructive pulmonary disease (COPD) and chronic heart failure (CHF) is also expanding.
The elderly population is rapidly growing, while lifespans also increase. At the same time, the prevalence of chronic obstructive pulmonary disease (COPD) and chronic heart failure (CHF) is also expanding.
In Sweden, the prevalence of heart failure among people age 80 or older is currently estimated at 10 percent while the prevalence of COPD is 8 percent among those aged 50—and increases by age.
Exacerbations of their condition without early treatment intervention often land elderly patients with advanced stages of COPD or CHF in the emergency room and/or hospital. CHF patients often are relieved of their condition through a combination of fluid restriction and diuretics, while moderate and severe exacerbation of COPD often is associated with an inflammatory response in the respiratory tract to an infection and demands antibiotics alone or a combination of antibiotics and steroids.
To gauge the effects of patient education and remote-based care technology on outcomes, researchers in Europe recently set about to determine if telemonitoring supported by hospital-based home care (HBHC) could detect exacerbations early and reduce the number of hospitalizations for patients with these conditions.
Researchers said that during the previous 15 years, a growing number of telehealth studies and reviews have included patients with CHF and/or COPD. Some of these studies have shown reduced morbidity and mortality, as well as positive effects on exacerbation and hospitalizations. However, to become successful, the introduction of a new home telemonitoring system in healthcare needs to be accepted by professional caregivers and their patients.
The most common barrier to telehealth tools was that patients had “no interest” and thought that the technology was too complicated. Considering this lack of familiarity to internet use, researchers employed a telemonitoring system—the Health Diary—based on digital pen technology. In a previous pilot study utilizing the digital pen technology, exacerbations of CHF were detected early, treatment was initiated at home by a specialized hospital-based home care unit, and hospitalization was avoided. In fact, none of the included subjects were hospitalized during the surveillance period of 13 months.
Considering the disease characteristics of CHF and COPD, researchers hypothesized that subjects in an HBHC setting of fragile, elderly patients with advanced stages of CHF or CPOD would exhibit differences regarding exacerbation frequency and subsequent need of healthcare. They set about to determine the healthcare utilization of elderly, sick patients with frequent hospitalizations, and which condition might dominate the need for care.
Additionally, patients with the most advanced form of COPD commonly present with right-heart failure. Primary outcome was exacerbation frequency and home healthcare contacts appearing during the intervention, thus, comparing COPD and CHF subjects. Secondary outcome was the number of hospitalizations during a one-year intervention, compared to the number of hospitalizations of the same subjects the one-year prior inclusion.
The causes behind hospitalization, whether urgent or planned, were of interest, as were the subjects’ experiences handling the technology, their participation in their own care, and heir knowledge of the illness and their feelings of security. Ninety-four patients with advanced diseases were enrolled (36 COPD and 58 CHF subjects) of which 53 subjects (19 COPD and 34 CHF subjects) completed the one-year study period. Death was the major reason for not finalizing the study. Compared to the one-year prior inclusion, the telehealth intervention significantly reduced hospitalization. Although COPD subjects were younger with less comorbidity, exacerbations and HBHC contacts were significantly greater in this group.
Thus, COPD subjects exhibit exacerbations more frequently, mainly because of disease characteristics, thus, demanding much more HBHC.
COPD Associated with Poorer Survival in Patients With NSCLC
 Researchers have found that the impact of pre-existing chronic obstructive pulmonary disease (COPD) in patients with non-small cell lung cancer (NSCLC), that COPD is associated with shorter survival and marked differences in early stages of lung cancer.
Researchers have found that the impact of pre-existing chronic obstructive pulmonary disease (COPD) in patients with non-small cell lung cancer (NSCLC), that COPD is associated with shorter survival and marked differences in early stages of lung cancer.
Among the 66,963 patients diagnosed with NSCLC, the 22,497 with pre-existing COPD had poorer median overall survival (192 days) compared with patients without comorbid disease (206 days) and an 11 percent higher risk of death.
Median survival decreased among patients with COPD for all stages. The elevated risk of death associated with pre-existing COPD decreased with each stage of NSCLC; stage 1 patients had a 39 percent increased risk of death, stage 2 patients a 20 percent higher risk, stage 3 a 9 percent higher risk, and stage 4 patients had a 4 percent higher risk.
Older age, gender, race, comorbidity score and tumor grade were all significantly associated with higher risk of mortality.
“One potential explanation for worse prognosis of lung cancer patients with COPD could be because of inadequate cancer treatments, poor pulmonary function and lower quality of life,” researchers said. “Studies have also shown that COPD was an important predisposing factor for the development of respiratory-related complications and poorer long-term survival outcomes.”
The researchers relied on data from the Surveillance, Epidemiology and End Results-Medicare database, focusing on patients aged 66 years and older with COPD who were diagnosed with NSCLC at any stage between 2006 and 2010, and those individuals who were continuously enrolled in Medicare parts A and B in the 12 months prior to diagnosis.
The researchers determined that those with chronic bronchitis had a more significant impact on time-to-death compared with emphysema for all stages of cancer.
The increased risk of death associated with chronic bronchitis compared with emphysema followed similar patterns seen among the COPD and non-COPD cohorts, with risk of death decreasing with each stage of NSCLC. Stage 1 patients had a 40 percent higher risk of death, stage 2 had a 28 percent higher risk, stage 3 a 10 percent higher risk, and stage 4 patients had a 6 percent higher risk.
Click here to read the full article on AJMC.
Living With COPD: Tips
 For those people who struggle with chronic obstructive pulmonary disease (COPD), the simple act of breathing can be a struggle. For many, COPD becomes a way of life, so steps must be taken to manage it.
For those people who struggle with chronic obstructive pulmonary disease (COPD), the simple act of breathing can be a struggle. For many, COPD becomes a way of life, so steps must be taken to manage it.
COPD affects more than 16 million Americans, according to the Center of Disease Control and Prevention. However, millions more have COPD, but have not been diagnosed and are not being treated.
Symptoms of COPD include frequent coughing or wheezing, excess phlegm or sputum and shortness of breath. Adults who have COPD are more likely to be unable to work and have trouble with daily activities—symptoms that can be exacerbated for those who smoke and who aren’t physically active.
The impacts of COPD affect a person’s day-to-day life enormously, and they must be addressed. Per the CDC, one in four adults with COPD say they are not able to work while others are forced to miss work because of symptoms. Additionally, half of adults with COPD say they limit their activities because of health problems, and more than 33 percent say they have trouble walking or climbing stairs. Finally, long-term medical costs tend to be higher for adults with COPD than those without.
Mitigating COPD impacts
There are things that individuals can do to make living with COPD easier. The most important is to quit smoking, if you are. If help is needed, speak with your doctor. There are solutions that may be able to help you in your journey to help you breathe easier.
Secondly, ask your doctor about participating in pulmonary rehabilitation. It is a personalized treatment program – as mentioned above – that is designed to manage COPD symptoms to improve quality of life. For example, these plans may include learning to breathe better and conserve physical energy, and may include specific advice regarding the best foods and exercise.
Nearly important as participating in a pulmonary rehabilitation program is properly taking medications, which can help control symptoms such as coughing or wheezing.
Finally, though it is not really something an individual can control, try to avoid lung infections, which can cause serious problems in people with COPD. The CDC recommends some vaccines, such as flu and pneumonia, for people with COPD.
Takeaways for Primary Care Physicians Treating COPD
 Chronic obstructive pulmonary disease (COPD) is complicated and requires intensive and specialized treatment, more so than some may have previously thought. That’s according to University of Pittsburgh investigators who
Chronic obstructive pulmonary disease (COPD) is complicated and requires intensive and specialized treatment, more so than some may have previously thought. That’s according to University of Pittsburgh investigators who
Decreasing and withdrawing from inhaler use should also be conducted an analysis of the current literature to synthesize the discussion about the current diagnosis and treatments for COPD.
In their brief, the researchers wrote that 30 million adults in the U.S. have COPD, and most of these patients have been diagnosed by a primary care physician—despite the complicated and specialized nature of the disease.
The study, “Diagnosis and Outpatient Management of Chronic Obstructive Pulmonary Disease,” was published in JAMA. In it, investigators identified 90 applicable studies and, from those, 26 included clinical trials, 21 were meta-analyses, 25 were observational studies and 18 included guidelines and other reports.
The authors of the new study found that the primary risk factor for COPD diagnosis is tobacco smoke. They did note that other exposure to inhaled particles, such as indoor cooking or smoke from wood and other fuels, could also play a role.
Researchers noted that a patient’s misuse of inhaler devices for COPD pharmacotherapy is “both incredibly common and oftentimes unnoticed by healthcare providers.” Additionally, the authors believe that better screening for and correcting improper use of inhalers could lead to improved disease control and reduced care costs.
Craig Riley, MD, lead researcher of the review, told MD Magazine, “An inordinately large number of patients are either diagnosed presumptively without spirometry (and may not have COPD) or are diagnosed with other conditions (and may not have them) despite having exposures and symptoms consistent with possible COPD. Incorrect diagnoses lead to incorrect and ineffective treatments.”
Riley noted that people’s understanding of how inhaler devices work should allow providers to screen patients for proper use. Likewise, if a patient is unable to adequately draw medication into their lungs, they will not see a benefit and are at higher risk of clinical deterioration.
considered, especially in patients who are able to maintain stability of two years or longer without a moderate to severe exacerbation of symptoms.
Pulmonary rehabilitation has a greater comparative benefit on COPD symptoms, hospitalizations and death than pharmacotherapies, Riley said. He also noted that a majority of COPD patients are never made aware of these pulmonary rehabilitation programs, which are meant to combine strength and endurance training with educational, nutritional and psychosocial support. As well, the programs are designed to help patients improve cardiovascular fitness, physical activity levels and symptoms in COPD patients.
“Greater availability and utilization of pulmonary rehabilitation has the potential to improve quality of life, decrease hospitalization costs and has been suggested to improve mortality following hospitalization,” Riley said.
Traveling with COPD
 Long-distance travel doesn’t have to be an impossibility for those living with chronic obstructive pulmonary disease (COPD). While just thinking about travel can be stressful, doing so is an achievable goal with proper preparation.
Long-distance travel doesn’t have to be an impossibility for those living with chronic obstructive pulmonary disease (COPD). While just thinking about travel can be stressful, doing so is an achievable goal with proper preparation.
Talk to your doctor
The first thing on your pre-travel check list should be a trip to your doctor to make sure they are fully aware of your plans and can guide you in your preparations. Also, your physician can ensure that you have enough medication for the journey and can get your prescriptions topped off ahead of time, so you don’t run out or encounter any unneeded stress related to medications along the way. You should also make sure to carry extra doses with you in case there are delays.
Seeing your doctor may also help assuage any of your own fears. Travel can be stressful when you have a medical condition and your doctor can help ease your mind. Before you make any plans, it’s best to ask if it’s safe for you to travel. Also, consider asking for any specific COPD-related travel tips. If you are traveling to a higher elevation than you’re used to, you’ll want to find out if you need to carry oxygen. And, in case of a worst-case scenario, you’ll want to know which healthcare facilities in the area are best for your condition. You might also want to ask for a portable version of your medical record—just in case.
In all cases, if you use supplemental oxygen, plan to bring extra tanks and extra nasal cannulas.
Travel by air and boat
If traveling by air, contact the airline in advance of the departure date regarding policies for oxygen. While personal portable oxygen concentrators can be taken aboard many airlines with advance notice, you may need a letter from the doctor, brief medical history and a current prescription. If you’re told that oxygen use is forbidden, contact the airline’s services for people with disabilities department to discuss your needs. Finally, keep your medications in your carry-on luggage.
For cruise ships, the same strategies often are applied. If you let the company know about your needs in advance, cruise line companies often can accommodate you.
Travel by bus and train
Like airlines, contact bus and train lines before you travel to explain that you’ll have oxygen. Most bus and train companies allow oxygen onboard without any trouble.
Travel by car
On road trips, don’t smoke in the car or allow any other passengers to do so as oxygen is highly flammable. Take ample breaks from the driving and plan your route to avoid high-traffic areas and times of heavy road congestion. Keep your oxygen upright in the seat next to you and, if you can, secure it with a seatbelt. Carefully, store extra oxygen tanks on the floor behind the front seat.
Traveling alone?
If you have plans to travel, it may be better to do so with a loved one or friend. When you travel together, you’ll likely feel more at ease and have a better chance to enjoy yourself.
That said, there is no one that knows your health better than you. If you don’t feel well at any point, try to take some time to relax or de-stress. If things get worse or you feel you need medical care, seek a doctor immediately.
Final tips
Per the Cleveland Clinic, prior to any pre-planned travel, call your home healthcare company and tell them where you’re going and how you’re getting there. They can help you arrange for oxygen when you arrive. Make sure you understand how your portable oxygen system works, including how long the oxygen will last.
There may be a fee related to oxygen use, so contact the travel lines ahead of time to check.
Finally, vacations can be great fun, and COPD conditions shouldn’t hold you back if you’re able to partake in one. If you take the proper precautions and prepare in advance, there’s likely nothing to worry about – except having fun!
Emphysema Might Increase Risk of Aneurysms
 While the how’s and why’s of why aneurysms develop are not well understood, a recent study indicates that those with chronic obstructive pulmonary disease (COPD) are at higher risk. The study, published in the American Heart Association journal Stroke, found that the risk an aneurysm will rupture is much higher for those with COPD, and suggests that COPD may be a marker to determine if someone is at a heightened stroke risk.
While the how’s and why’s of why aneurysms develop are not well understood, a recent study indicates that those with chronic obstructive pulmonary disease (COPD) are at higher risk. The study, published in the American Heart Association journal Stroke, found that the risk an aneurysm will rupture is much higher for those with COPD, and suggests that COPD may be a marker to determine if someone is at a heightened stroke risk.
Aneurysms develop on the wall of the aorta, which supplies blood to the abdomen, pelvis and legs. If one ruptures, it creates a life-threating situation. Researchers posit that the damage done by emphysema to the alveoli sacs in the lungs increase the risk for rupture. This conclusion was made after analyzing data for about 1.7 million Medicare beneficiaries over the age of 65, then following them for an additional four years. Of the more than 4,800 patients diagnosed with an aneurysm rupture, 433 had emphysema.
After accounting for other risk factors—hypertension, diabetes, tobacco use and alcohol abuse—researchers found that people with emphysema were more than twice as likely to experience a ruptured aortic aneurysm. They were also 50 percent more likely to have a subarachnoid hemorrhage caused by their aneurysm.
"We [should] tell patients with emphysema that they are at higher risk for aneurysm formation, screen them and work with them on modifiable risk factors like smoking and blood pressure control," said Dr. Ali Mahta, the study's lead author and an assistant professor of neurology in the Warren Alpert Medical School of Brown University in Providence, RI.
The study, which is the largest of its kind on the topic of aneurysm and emphysema, also suggests the two conditions may share a similar underlying pathology, accounting for their relationship, said Mahta.
The study doesn’t prove the correlation, of course, and there are limitations. For example, the study does not capture clinical variables such as severity, treatment or duration of a patient's emphysema or aneurysm, or the context in which the diagnosis was made. Even though smoking is a factor of both conditions, the data here did not show if those studies were smokers.
To read the full article on Health Day, click here.
Spreading Awareness of the Risk of Lung Cancer in Patients with COPD
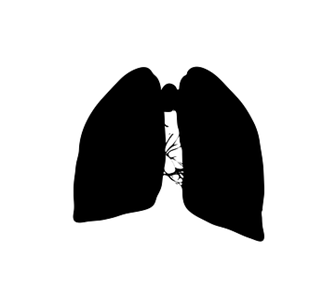 Most patients with COPD require greater motivation to seek help when symptom changes occur and most people are unaware of their increased risk of developing lung cancer, according to new research.
Most patients with COPD require greater motivation to seek help when symptom changes occur and most people are unaware of their increased risk of developing lung cancer, according to new research.
In a UK-based qualitative interview study published in Psycho-Oncology, researchers explored how COPD affects patient response to changes in their symptoms and sought to explain their reluctance to seek help from medical professionals. The results showed that patients often disregarded early signs of lung cancer and instead believed they were COPD-related. They also showed that none of the patients knew about the link between their condition and the potential onset of lung cancer.
“Various factors were considered to explain why patients avoided seeking medical treatment,” the researchers said. “Researchers acknowledged awareness to the risk of lung cancer, prompt diagnosis, and early treatment could prolong survival rates.”
Between July 2016 and May 2017 interviews were completed with 40 patients with COPD aged 40 to 83 in Glasgow, Scotland. Questions were related to four different “circles of influence” regarding patient self-knowledge, his or her amount of social interaction, cultural attitudes and social structure.
Researchers were able to gather information on each patient’s symptom experience, interpretation, action, recognition, help-seeking tendencies, evaluation and re-evaluation. Likewise, cultural influences had a dramatic effect on individuals’ reluctance to seek professional help.
“Many participants wanted to be considered ‘good patients’,” researchers said.
For example, patients felt concern about wasting a physician’s time, which demonstrates mindfulness of a moral balance between responsible use of medical services and avoidance of needlessly sacrificing their health.
“Many patients emphasized they would only consult their physician in critical circumstances,” the research found.
Patients also were more likely to be fatalistic and were deterred from seeking care. In fact, a number of individuals interviewed said they felt pessimistic about the idea of achieving improved symptoms. Social interaction also was a key influence on an individual’s likelihood to seek treatment. For example, family members and friends noticed worsening coughs or physical changes when patients failed to recognize any change themselves. Those who had the support of family or friends had a greater chance of attaining help than those who expressed feelings of isolation.
Social capacity was also found to be a major influencer on a patient’s tendency to seek help. Many patients said they purposefully avoid social situations that could alert others to their condition because of their feelings of embarrassment about it. In addition to social isolation, other barriers to care included scheduling appointments beyond typical working hours and transportation or physical mobility issues.
The prevalence of lung cancer, which is among the most common forms of cancer, is four times higher in patients with COPD. Researchers indicated concern that informing patients of a link between COPD and cancer could be harmful and lead to increased fatalism, but also said that raising awareness of the relationship between “COPD and lung cancer will enlighten patients to the benefits of early diagnosis.”
“Healthcare professionals need to do more to educate those with COPD about their increased risk of developing lung cancer and be more vigilant when a patient with the illness presents changing symptoms,” said Kathyrn A. Robb, PhD, and senior lecturer at the University of Glasgow, in a statement.
Know the Warning Signs of COPD
In the beginning stages of chronic obstructive pulmonary disease (COPD), patients may have no symptoms – or have only mild ones. But as the disease progresses, symptoms may include chest tightness, a cough with mucus, low fever, shortness of breath and wheezing. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) no longer emphasizes distinguishing chronic bronchitis from emphysema, the two main types of COPD. It instead focuses on the airflow-limited state.
 That said, COPD is a disease that includes persistent respiratory symptoms accompanied by airflow limitation that is secondary to airway and/or alveolar abnormalities, often caused by significant exposure to noxious gases or particles. Chronic bronchitis is defined as the presence of cough and sputum production for at least three months a year in each of two consecutive years, according to GOLD’s 2019 report.
That said, COPD is a disease that includes persistent respiratory symptoms accompanied by airflow limitation that is secondary to airway and/or alveolar abnormalities, often caused by significant exposure to noxious gases or particles. Chronic bronchitis is defined as the presence of cough and sputum production for at least three months a year in each of two consecutive years, according to GOLD’s 2019 report.
Patients with chronic bronchitis and emphysema may be differentiated by their presentation, including associated cardiac and lung assessment findings, sitting position in the office, type of cough and weight. Those with chronic bronchitis may be obese and experience frequent coughing with expectorant, coarse rhonchi and wheezing on lung exam, and edema and cyanosis that can be associated with right-sided heart failure. They also may be thin and have barrel chests.
Hyper-resonant lung sounds and wheezing may be heard, or they may have pursed lip-breathing accompanied by a tripod position and use of accessory muscles and little or no cough or expectorant reported.
COPD diagnosis is made with spirometry, when the ratio of forced expiratory volume in one second is less than 70 percent of a match control, signifies an obstructive defect. A high-resolution computed tomography can help diagnose emphysema, given that it has better sensitivity then a chest radiograph.
The six-minute walk test is part of the BODE index (Body-mass index, airflow Obstruction, Dyspnea, and Exercise) to predict mortality for patients with COPD. There are other tests, of course. Differential diagnosis of COPD can include asthma, bronchiectasis, congestive heart failure, diffuse pan bronchiolitis, and obliterative borchiolitis.
The key to managing COPD is a thorough assessment that includes spirometry testing, the nature and magnitude of the symptoms, history of moderate and severe exacerbations and future risk, and presence of comorbidities, such as diabetes, gastroesophageal reflux disease, heart failure and osteoporosis.
The GOLD (2019) refined ABCD assessment tool can then be used to guide treatment, the goals of which include improving exercise tolerance and health status, preventing disease progression, preventing and treating exacerbations, reducing mortality and relieving symptoms. Smoking cessation is key to managing chronic bronchitis and COPD.
Treatment includes medications, such as inhaled or oral corticosteroids, short- and long-acting bronchodilators, phosphodiesterase, inhibitors, respiratory anticholinergics and a combination medication and corticosteroids or anticholinergic inhalations. Treatment may also include improved diet, infection control, management of sputum viscosity and clearance, oxygen therapy, pulmonary rehab, smoking cessation, vaccinations and anti-trypsin deficiency treatment to aid the patient’s functional status and quality of life.
Chronic bronchitis is the beginning point of the progression of COPD. Research is being done to analyze mucin concentration and phlegm samples, as well as clinical trials for patients with chronic bronchitis by attempting to kill cells that produce mucus with low-level energy.
Researchers breathe new life into COPD research using mouse models
 Researchers at Tokyo Medical and Dental University (TMDU) used mice to demonstrate that immune cells called basophils act to trigger a cascade of immune responses leading to airway degeneration resembling that in human chronic obstructive pulmonary disease (COPD).
Researchers at Tokyo Medical and Dental University (TMDU) used mice to demonstrate that immune cells called basophils act to trigger a cascade of immune responses leading to airway degeneration resembling that in human chronic obstructive pulmonary disease (COPD).
In the study, published in the journal Proceedings of the National Academy of Sciences USA, researchers used a variety of mouse models to explain the developmental process behind COPD. The team showed that the immune cells basophils, previously believed to be mainly involved in fighting parasitic infections and inducing allergic responses, also induce the destruction of alveolar walls (emphysema).
“Earlier studies of COPD focused on mice as a suitable model for easily dissecting the mechanisms behind this disease, but encountered a range of difficulties in mimicking the features in humans,” the researchers noted.
Per reports on the study, the mice were first exposed to smoke, given the association between smoking and COPD, but there was no measurable “progressiveness of the disease in humans.” Next, researchers administered enzymes called proteases directly into the airway. Proteases break up proteins, producing more human COPD-like features.
They were able to induce emphysema in mice. Lead author, Sho Shibata, said the team then worked backwards one step at a time through the series of events causing this symptom to identify what started this cascade, using mice to knockout of each component of this cascade.
“The team started by revealing that the lung tissue destruction was caused by a molecule called MMP-12, which they found was released in excess from immune cells called interstitial macrophages when elastase was administered,” Science Daily reported.
By working backward, the researchers said they found “interstitial macrophages arose when the precursor immune cells called monocytes were induced by an immunity-regulating molecule called interleukin-4,” thus showing that this interleukin-4 was released by the immune cells basophils.
Ultimately, they were able to treat the mice that elicited emphysema.
"Our results are surprising because basophils have not previously been identified to be active in this kind of situation," said corresponding author Hajime Karasuyama. "It may be that basophils were previously overlooked because they only make up 1 percent of the white blood cells in the lungs."
The team hope that their discovery will lead to therapies targeting basophils or the interstitial macrophages that they create to slow down the progression of emphysema.
Diet for COPD sufferers
 Living with chronic obstructive pulmonary disease (COPD) requires more than a few adjustments to help the afflicted conserve energy and optimize lung function. Two adjustments should be eating well and maintaining a healthy weight, which may help keep symptoms in check and let COPD suffers live a more high-quality and active life.
Living with chronic obstructive pulmonary disease (COPD) requires more than a few adjustments to help the afflicted conserve energy and optimize lung function. Two adjustments should be eating well and maintaining a healthy weight, which may help keep symptoms in check and let COPD suffers live a more high-quality and active life.
“If you're overweight, you have to carry more of your weight around, making you feel more short of breath,” Barry Make, MD, co-director of the COPD program at National Jewish Health in Denver and a professor of medicine at the University of Colorado Denver, School of Medicine, told Everyday Health.
Nutrition Tips
Before beginning any diet, speak with your medical team about the nutrition plan that is best for you related to your specific body and health factors. A nutritionist may be required, who can help develop a meal plan to best meet your needs and monitor progress along the way.
However, in general, people who have COPD should consider the following to maintain an optimal weight:
-
Monitor calories: The American Lung Association (ALA) recommends that people with COPD who are overweight consume fewer calories. If the opposite is true and you need to focus on maintaining or increasing your body weight, talk with your medical team or nutritionist about the foods you should be eating to keep the weight on.
-
Avoid fad diets: Fad diets are not appropriate for COPD patients. People with COPD appear to fare best with a varied diet that provides a good balance of whole grains, fruits, vegetables and lean proteins, according to research published the International Journal of Chronic Obstructive Pulmonary Disease.
-
Focus on protein: Protein is particularly important for COPD patients who are exercising as part of their pulmonary rehabilitation plan. The ALA recommends milk, eggs, cheese, meat, fish, poultry, nuts and beans as good protein sources.
-
Watch your portions: Consider eating small meals frequently, rather than fewer large meals. Eating throughout the day instead of two or three large meals can help lessen shortness of breath.
-
Get balanced: Focus on consuming fruits, vegetables, dairy products, whole grains and lean proteins.
-
Limit salt: Consuming excessive sodium can lead to fluid retention, which can worsen shortness of breath.
A healthy diet is an important part of a COPD treatment plan. It can also help manage symptoms, and make people feel better overall by potentially increasing their energy level and giving their body the fuel needed to fight infection.




